A research assistant prepares a PCR reaction for polio at a lab at Queens College on August 25, 2022, in New York City.
Angela Weiss | AFP | Getty Images
When a young adult in a New York City suburb visited an emergency department in June after experiencing weakness in their lower legs, the shocking diagnosis would lead local officials to declare a health emergency in New York and put authorities across the U.S. and around the world on a state of alert.
The individual, a resident of Rockland County, had suffered from a fever, a stiff neck, back and abdominal pain as well as constipation for five days. The patient was hospitalized and tested for enterovirus, a family of pathogens that in rare cases can cause weakness in the arms and legs.
New York state’s Wadsworth Center and the Centers for Disease Control and Prevention would subsequently confirm the worst: The young adult was suffering from paralysis after contracting polio, the first known U.S. case in nearly a decade and the first in New York since 1990.
The patient was unvaccinated.
“I was very surprised. I never thought I’d see a case of polio in the United States, certainly not in Rockland County,” said Dr. Patricia Schnabel Ruppert, the county health commissioner. The CDC considers a single case of paralytic polio a public health emergency in the U.S.
Polio is a devastating, incurable disease that once struck fear into parents’ hearts every summer when transmission peaked, threatening children with paralysis. But the virus has faded from U.S. public consciousness over the decades after a successful vaccination campaign crushed transmission in the 1960s.
In the late 1940s, more than 35,000 people were paralyzed from polio in the U.S. every year, according to the CDC. But the advent of an effective vaccine in 1955 dramatically reduced the spread of the disease to less than 100 cases annually by the 1960s.
The virus had been eliminated from the U.S. by 1979, though sporadic cases that originated abroad have been identified over the years.
Digitally generated image of 3D molecular model of polio virus
Calysta Images | Tetra Images | Getty Images
How polio reemerged in New York this year remains the subject of investigation, but public health officials believe the virus originated overseas in a country that still uses the oral polio vaccine. American health officials stopped using the oral vaccine more than 20 years ago because it contains live virus that can — in rare circumstances — mutate to become virulent, but it is still common in other countries.
Genetic analysis of New York poliovirus samples indicates a weakened virus strain used in one of the oral vaccines mutated over time to cause the outbreak. Combined with low vaccination rates in some New York communities and greater international travel, this provided an opening for the virus to slip back into the U.S. this year and paralyze the Rockland patient.
“The underlying lesson is this is an infectious disease and it travels easily with population movements,” said Oliver Rosenbauer, a spokesperson for the Global Polio Eradication Initiative, the organization that represents the worldwide campaign to eliminate the virus.
Vaccine-derived virus
The oral polio vaccines are generally safe, effective, cheap and easy to administer. They have played a crucial role in the global campaign to eradicate polio, one of the most ambitious public health initiatives since smallpox was successfully stamped out in 1980. Two of the three naturally occurring poliovirus strains, called wild types, have been eradicated in the 21st century.
As recently as 1988, polio paralyzed 350,000 children annually across 125 countries, according to data from the polio eradication initiative. Today, Pakistan and Afghanistan are the only countries in the world where the remaining wild type polio is still endemic, with 27 cases confirmed so far this year. The annual number of wild poliovirus cases has declined by 99% since 1988.
The global fight against polio has relied on the oral vaccine’s ability to block transmission of the virus. The oral vaccine uses a live but weakened form of poliovirus that replicates in the gut. This builds immunity in the intestines that can block the virus from shedding in human feces and contaminating the environment.
Although recently immunized people can pass the oral vaccine virus on to others for a few weeks, it’s not normally a problem because the strain is weakened so it does not cause disease, Rosenbauer said. When the weakened virus from the vaccine spreads from person to person, it can actually help build immunity in a community, he said. The transmission eventually burns out once enough people have immunity, he said.
The problem begins when immunization rates are so low in a community that the weakened virus from the vaccine spreads uninterrupted for a prolonged period and mutates into a virulent strain, called a vaccine-derived poliovirus. And when people who are not immunized catch the mutated vaccine-derived virus, they can become paralyzed, like the patient in Rockland County.
“This thing has now circulated and emerged into something different,” Rosenbauer said. “It’s linked to the vaccine, but it’s actually more linked to vaccination coverage, because it doesn’t happen overnight, it takes months for these amounts of changes to occur.”
Blood sample positive with polio virus
Jarun011 | Istock | Getty Images
New York has been struggling with dangerously low polio vaccination rates in some communities for years. In Rockland, the vaccination rate for children under age two dropped from 67% in 2020 to 60% in 2022, according to the CDC. In some areas of Rockland, only 37% of kids in this age group are up to date on their vaccine.
The U.S. uses an inactivated polio vaccine administered as a shot. The polio strains in the shots have been killed, meaning the virus cannot mutate into a more virulent form. The inactivated polio vaccine is very effective at preventing disease, but it does not stop transmission of the virus.
It builds immunity in the bloodstream, which prevents the virus from attacking the spinal cord and causing paralysis. But the inactivated vaccine does not stop the virus from replicating in the gut, which means transmission between people is still possible if there’s an outbreak.
This means that although people immunized in New York with the inactivated polio vaccine are protected against disease, they can still catch and spread the strain that mutated from the oral vaccine. This is likely what’s happening in New York right now, Rosenbauer said.
Polio’s silent spread in New York
Poliovirus has been spreading silently in New York communities for months. After the Rockland County patient developed paralysis, health officials in New York used wastewater surveillance developed during Covid to test sewage samples.
Poliovirus was detected in Rockland County, then in neighboring Orange County, New York City, Sullivan County and later in Nassau County on Long Island. The earliest positive sewage samples dated back to April in Orange County. Polioviruses have been found in 69 sewage samples in New York state so far.
While the Rockland County adult hadn’t traveled internationally, they attended a large gathering eight days before they started experiencing symptoms, which suggests that they had contracted the virus from someone else in the community, Schnabel Ruppert said.
Most people who catch polio don’t show symptoms, while about 1 in 4 people infected have a mild illness similar to the flu. Paralysis occurs in one out of every 200 or one out every 2,000 people who catch the virus, depending on the strain. The identification of even a single paralytic case is an alarm bell that indicates the virus has been spreading widely in the community.
“When we see one case of paralytic polio, that means there are probably hundreds and hundreds of cases that are out there in the community but not diagnosed, because 75% of the cases are asymptomatic,” Schnabel Ruppert said.
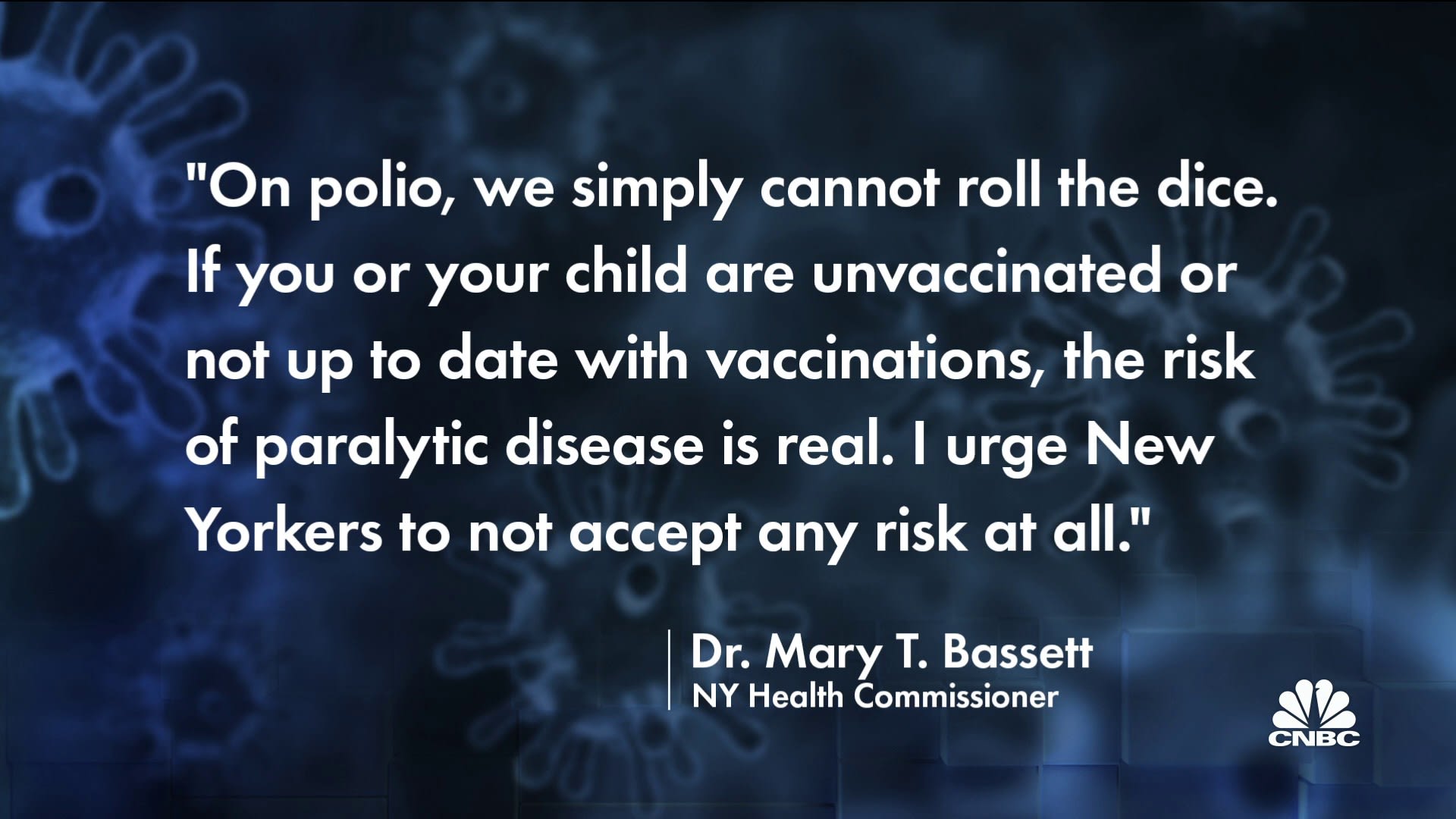
The Rockland County health commissioner said she’s very concerned another unvaccinated person in the community could contract paralytic polio. New York Gov. Kathy Hochul declared a state of emergency last month with the goal of boosting the statewide vaccination rate, which currently stands at 79%, to well above 90% to prevent a future outbreak.
New York Governor Kathy Hochul speaks at a news conference on August 03, 2022 in New York City.
Spencer Platt | Getty Images
New York Health Commissioner Dr. Mary Bassett on Wednesday declared the poliovirus outbreak an imminent threat to public health.
“We know that there’s still circulation actively in communities here. And we know that there’s still unvaccinated pockets of the population. And so we’re still worried,” said Dr. Eli Rosenberg, one of the leading state public health officials working on New York’s response to the outbreak.
The London and Jerusalem connection
New York isn’t the only polio-free place where the virus has reemerged this year. Poliovirus has also been detected in wastewater in London and Jerusalem. Fortunately, there are no known cases of paralysis in either city, though the U.K. health authorities declared a national incident after detecting the virus.
Israel eliminated polio in 1988 and the U.K. did so in 1982, according to the polio eradication initiative.
The New York poliovirus samples are genetically linked to the specimens found in London and Jerusalem, according to the group. The viruses in all three countries are related to the weakened Sabin Type 2 virus used in one of the oral polio vaccines.
The U.K., like the U.S., does not use oral vaccines at all, and Israel does not use oral vaccines containing the Sabin Type 2 strain, according to the initiative. And the poliovirus samples from the three countries are not linked to known vaccine-derived polio virus outbreaks in other countries, such as the Democratic Republic of the Congo, Nigeria, Somalia and Yemen, Rosenbauer said.
Girl receives anti-polio vaccination drops.
Ramesh Lalwani | Moment | Getty Images
This suggests that someone from a country that still administers the oral vaccine containing Sabin Type 2 traveled to Israel, the U.K. or the U.S. and seeded the weakened virus there, Rosenbauer said. It then mutated at some point to become more virulent, but it’s unclear whether this evolution occurred in Israel, the U.K. or the U.S., he said.
Israel and the U.K. have detected poliovirus in sewage samples dating back to January and February, respectively, well before the earliest known U.S. specimen was detected, in April, according to the World Health Organization.
The CDC, in a statement, said although the Rockland County patient did not travel to a country where vaccine-derived virus is present, it’s possible others in the individual’s community may have visited such a place or a visitor brought it into the U.S.
Steve Oberste, who heads the CDC’s polio lab, said genetic analysis of the sample from the Rockland patient indicates the virus is about a year old. The links between the specimens in Israel, the U.K. and the U.S. point to some movement between the three countries that spread the virus, Oberste said, but there’s no way to determine the direction of the transmission between the countries.
It’s difficult to trace the epidemiology since the patient didn’t travel, the mutations in the viruses are small and international travel in and out of New York is heavy, he said.
“With a single case there’s no way to know exactly how many infections there were between the vaccine vial and the paralyzed person,” Oberste said.
It’s unlikely public health authorities will figure out the origin of the virus that paralyzed the patient in New York, Oberste said. Dozens of countries around the world — primarily in Africa, the Middle East and South Asia — are still using oral vaccines that contain the Sabin Type 2 strain.
The vaccine virus is the same in every vial, so there’s no identifying feature on it that would allow scientists to trace wastewater specimens found in New York back to a specific country that still uses the oral vaccine containing the Sabin Type 2 strain, Oberste said.
“This started its journey somewhere else on Earth. Where on Earth is very hard to say. But there were mutations that were accumulated across probably successive waves of transmission from person to person to person and landed unfortunately with an unvaccinated resident of Rockland County,” Rosenberg said.
Outbreak risk
The Rockland County adult is the sole paralytic case so far, but the risk of more unvaccinated people developing severe disease is real. In 1992, wild type poliovirus found its way into a community in the Netherlands that refused vaccination for religious reasons, which resulted in 59 cases of paralysis and two deaths.
New York state health officials have repeatedly called on parents to immediately start the vaccination series for their children if they haven’t already and for unvaccinated adults to do the same. Most adults in the U.S. are assumed to have protection against polio because the overwhelming majority of people are vaccinated when they are children, according to the CDC.
Health authorities in New York, Israel and the United Kingdom have all responded swiftly to prevent an explosive outbreak of polio like the one in the Netherlands 30 years ago, Rosenbauer said. The arrival of fall and winter in New York and London should also help slow transmission, because polio doesn’t spread as efficiently in colder weather, he said.
An anonymous survivor of polio pushes the handrims of his wheelchair.
Michael Edwards | Istock | Getty Images
“Hopefully, we will have a situation where the sanitation infrastructure is sufficiently strong, vaccination coverage is sufficiently strong, and disease surveillance is sufficiently strong to where the virus stops circulating again,” Rosenbauer said.
The goal of the Global Polio Eradication Initiative is to switch the world to the inactivated vaccine once the oral vaccine has stamped out the remaining wild type poliovirus. This switch would eliminate the risk of vaccine-derived virus outbreaks.
But making the switch will be a difficult needle to thread. The oral polio vaccine is needed to eradicate wild type virus from the world, but it also carries the risk of mutating into a virulent form. And when vaccine-derived virus outbreaks happen, the oral vaccine is used to stop them — even in countries that rely on the inactivated vaccines for routine immunization, according to the CDC.
In Rockland County, more than 6,400 doses of the inactivated vaccine have been administered so far this year and about 64% were given in the two ZIP codes with the lowest immunization rates for kids under age two, Schnabel Ruppert said. But there’s still a long road ahead to achieve a vaccination rate of more than 90%, she said. Children need four doses of the vaccine, and unvaccinated adults need three.
“This is a long process. For each person, it’s going to take months and months in order to get them vaccinated, to catch up,” Schnabel Ruppert said.
Rosenberg said while receiving the entire vaccination series is crucial, the biggest jump in protection against severe disease and death comes with the first dose, which is why it’s so important for unvaccinated people to get their first shot now.
Rosenbauer said the question is whether immunization campaigns with the inactivated vaccines in New York and London are enough or whether the oral vaccine might need to be temporarily reintroduced to break the chain of transmission.
The CDC, in a statement, said it is not changing its recommendations on the use of the inactivated polio vaccine at this time. Polio is not endemic in the U.S., and vaccination coverage remains high at more than 92% nationwide, according to the CDC.
This article was originally published on CNBC